Phenylephrine HCl is a direct-acting synthetic sympathomimetic that selectively stimulates α-1-adrenergic receptors, producing rapid peripheral vasoconstriction and a predictable rise in systemic vascular resistance. The injectable formulation is routinely chosen for the short-term management of clinically important hypotension during anesthesia, septic shock, or other states of vasodilatory collapse when cardiac output is judged adequate. In contrast with mixed α/β agonists, phenylephrine has negligible β-adrenergic activity, thereby minimizing chronotropic effects while providing potent arterial and venous tone. Because of these properties, clinicians value the agent’s ability to augment mean arterial pressure without directly increasing myocardial oxygen demand, provided that intravascular volume is optimized.
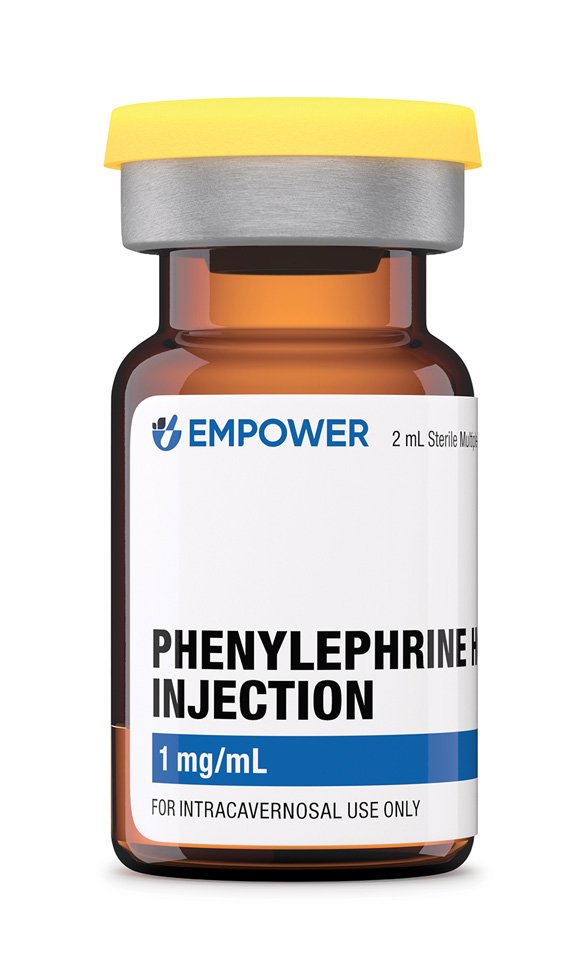
Each 2 mL vial contains 1 mg/mL phenylephrine HCl in water for injection adjusted to pH 3.0-5.0 with hydrochloric acid; no antimicrobial preservative is added. The solution is clear and colorless, intended for intravenous bolus or continuous infusion after dilution in compatible fluids. Compounding under section 503A affords flexibility in concentration and volume while obligating the prescriber and pharmacist to document clinical need and to counsel patients that, although the active moiety is listed in the United States Pharmacopeia, the compounded preparation itself has not undergone FDA pre-market approval.
For perioperative hypotension in adults with adequate cardiac function, an initial intravenous bolus of 50-200 µg may be administered over 20 seconds, repeating every 1-2 minutes as needed until target mean arterial pressure is achieved. Continuous infusion typically commences at 0.25-1.0 µg/kg/min, titrating by 0.1-0.2 µg/kg/min increments every 5 minutes, not to exceed 2 µg/kg/min in most settings. Critically ill patients may require higher rates subject to invasive hemodynamic monitoring. Pediatric dosing is weight-based (0.1-0.5 µg/kg/min) and mandates infusion pumps with micro-dosing capability. Solutions should be prepared in aseptic conditions: diluting 10 mg of phenylephrine in 100 mL of 0.9 % sodium chloride yields 100 µg/mL; lower concentrations (40 µg/mL) are recommended for peripheral lines. When discontinuing, taper gradually to avoid rebound hypotension.
Phenylephrine binds to post-synaptic α-1-adrenergic receptors located predominantly on vascular smooth muscle. Receptor activation triggers the phospholipase-C pathway, liberating inositol-1,4,5-trisphosphate and diacylglycerol, which in turn increase intracellular calcium from the sarcoplasmic reticulum and extracellular influx. Elevated cytosolic calcium complexes with calmodulin, activating myosin light-chain kinase, culminating in actin-myosin cross-bridge cycling and vasoconstriction. Systemic effects include increased systolic and diastolic pressures and reflex vagally mediated bradycardia. Cerebral and coronary perfusion pressures rise, yet regional blood flow distribution may vary with baseline autoregulation status; studies in anesthetized humans note preserved cerebral flow but potential reductions in cerebral tissue oxygen saturation, underscoring the importance of individualized hemodynamic targets.
Pharmacokinetically, intravenous phenylephrine displays a rapid distribution half-life of approximately 2-5 minutes and an effective plasma clearance dominated by sulfotransferase-mediated conjugation and oxidative deamination via monoamine oxidase. Hepatic metabolism is limited; the drug is extensively metabolized in the intestinal wall, kidneys, and other organs, with <20 % excreted unchanged. First-pass inactivation explains its low and variable oral bioavailability, whereas parenteral routes yield prompt onset (30-90 seconds) and brief duration (≤ 15 minutes after a bolus), making continuous infusion advantageous for sustained control.
Absolute contraindications include severe hypersensitivity to phenylephrine or any excipients and situations where vasoconstriction could exacerbate end-organ ischemia such as uncontrolled hypertension, thyrotoxicosis, or pheochromocytoma. Patients with occlusive vascular disease-coronary, cerebral, or mesenteric-face heightened risk of ischemic sequelae because α-1-mediated vasospasm may compromise collateral circulation. Ophthalmic literature documents myocardial infarction and cerebrovascular accidents after topical phenylephrine, highlighting systemic vulnerability even with local exposure, which extrapolates to parenteral dosing in predisposed populations.
Relative contraindications encompass narrow-angle glaucoma, severe aortic stenosis, and pulmonary hypertension. Reflex bradycardia can provoke decreased cardiac output in fixed-stroke-volume lesions, while increased afterload may worsen right ventricular failure. Case reports describe hypertensive urgency following dilute (2.5 %) topical administration, reinforcing that systemic absorption varies with mucosal integrity and comorbidities. Vigilant pre-procedure screening and blood pressure monitoring are imperative, and alternative pressors should be considered when myocardial ischemia or cerebrovascular autoregulatory failure is present.
Concomitant use with monoamine oxidase inhibitors (MAOIs) potentiates catecholamine pressor responses by inhibiting metabolic degradation, predisposing to severe hypertension; a 14-day washout is generally advised before elective procedures. Non-selective β-blockers may shift the hemodynamic response toward unopposed α-adrenergic vasoconstriction, exaggerating hypertension and diminishing cardiac output, whereas class III anti-arrhythmics warrant caution due to overlapping bradycardic effects. Over-the-counter cold remedies containing decongestants can synergize with phenylephrine; patients receiving serotonergic antidepressants have developed pressor crises attributable to cumulative adrenergic activity.
Halogenated inhalational anesthetics sensitize the myocardium to catecholamines but, with phenylephrine’s minimal β-activity, arrhythmogenic synergy is less pronounced than with epinephrine. Nevertheless, volatile agents may attenuate baroreflex, amplifying bradycardia and necessitating dose adjustment. Concurrent vasopressors such as norepinephrine or vasopressin may be co-titrated, but clinicians should monitor for excessive vasoconstriction leading to digital or mesenteric ischemia.
Common dose-dependent adverse effects are reflex sinus bradycardia, transient hypertension, and decreased renal or mesenteric perfusion secondary to elevated systemic vascular resistance. Cardiovascular complications include arrhythmias, myocardial ischemia, and, in rare instances, stress-induced cardiomyopathy; ocular studies combining phenylephrine with anticholinergics demonstrate additive tachycardia and hypertensive episodes, emphasizing polypharmacy considerations.
Vascular access site complications-extravasation, local ischemia, or necrosis-occur more frequently with peripheral administration of concentrated solutions. Meta-analytic data indicate serious tissue injury in < 2 % of cases when concentrations ≤ 40 µg/mL are infused through large-bore upper-extremity catheters, yet vigilance with frequent site inspection remains mandatory. Less common reactions include anxiety, tremor, pallor, and piloerection. Pulmonary edema has been reported in susceptible patients due to abrupt afterload increase.
Animal reproduction studies suggest dose-related fetal growth restriction and increased resorptions at exposures exceeding the human intravenous dose; phenylephrine crosses the placenta and may reduce uterine blood flow via vasoconstriction.
Human data are limited to case series and pharmacovigilance reports; the medication is classified as Pregnancy Category C, reflecting absence of controlled trials and the potential for harm weighed against clinical necessity.
Obstetric anesthesiology practice favors phenylephrine over ephedrine for treating spinal-induced hypotension during cesarean section because it maintains maternal blood pressure with lower fetal acidosis, yet careful titration and continuous fetal monitoring are recommended.
Store vials at controlled room temperature (20 – 25 °C) and protect from light by keeping them in their original cartons until use. Phenylephrine is stable under these conditions through the beyond-use date assigned after potency testing; exposure to ultraviolet light accelerates degradation, producing potentially inactive or irritant by-products. Do not freeze. Once the stopper is penetrated, use immediately and discard any unused portion to prevent microbial contamination.