Norditropin Injection is a sterile, preservative-free, recombinant human growth hormone (rh-GH) solution for subcutaneous administration. As a bioengineered analogue of endogenous somatropin, the formulation is designed to supplement or replace insufficient pituitary growth hormone secretion in pediatric and adult populations.
Clinically, Norditropin has been prescribed for growth hormone deficiency (GHD), short stature conditions such as Turner syndrome or children born small for gestational age without catch-up growth, and for adult-onset or childhood-onset GHD persisting into adulthood. The product remains a prescription-only agent; its safety and efficacy profile derive from published clinical trials of rh-GH and post-marketing surveillance rather than specific FDA approval for the compounded presentation.
Clinicians therefore must rely on peer-reviewed data, professional guidelines, and vigilant monitoring to balance potential benefits in linear growth, body-composition improvement, and metabolic regulation against known risks such as intracranial hypertension, musculoskeletal discomfort, impaired glucose tolerance, and neoplastic progression.
Initial dosing for pediatric GHD typically starts at 0.024-0.034 mg/kg daily administered subcutaneously 6-7 days per week, titrated to serum IGF-1 within the age-appropriate upper-normal range. Children with Turner syndrome, Noonan syndrome, or born small for gestational age without catch-up growth may require doses up to 0.067 mg/kg daily.
Adult GHD therapy often begins with 0.2 mg/day (approximately 0.004 mg/kg) and escalates by 0.1-0.2 mg increments every 1-2 months based on clinical response and IGF-1, not exceeding 0.016 mg/kg daily. Penetration of the needle into subcutaneous tissue rather than muscle optimizes absorption and minimizes lipoatrophy; rotation of injection sites (abdomen, thigh, upper arm, buttock) is mandatory. Dose omissions should be avoided, but if a partial week of therapy is missed, remaining doses should resume without doubling.
Somatropin exerts its physiological effects by binding to growth hormone receptors on target tissues, particularly hepatocytes, adipocytes, and chondrocytes. Receptor engagement activates the JAK2-STAT5 signaling cascade, triggering transcription of insulin-like growth factor-1 (IGF-1) and a host of IGF-1-dependent peptides that mediate longitudinal bone growth, nitrogen retention, and lipolysis.
Endocrine crosstalk is extensive: somatropin may antagonize insulin action via gluconeogenesis enhancement, yet it simultaneously reduces adiposity by stimulating hormone-sensitive lipase. In cartilage, local IGF-1 promotes matrix expansion and chondrocyte proliferation, accounting for epiphyseal plate widening in responsive children. In adults, the same pathways shift the ratio of lean to fat mass, supporting basal metabolic rate and cardiovascular structure.
Pharmacokinetically, subcutaneous rh-GH reaches peak serum concentrations in 3-6 h and is cleared hepatically and renally, with a terminal half-life of roughly 2-3 h; however, downstream IGF-1 elevations persist 12-24 h, permitting once-daily administration.
Therapy with compounded somatropin is contraindicated in patients with active malignancy, proliferative or severe non-proliferative diabetic retinopathy, acute critical illness following major surgery or respiratory failure, or hypersensitivity to the protein or formulation excipients.
Pediatric use is forbidden in individuals with closed epiphyses or in those with Prader-Willi syndrome who are severely obese or have significant upper-airway obstruction, owing to reported cases of sudden death. Clinicians should also defer treatment in the presence of uncontrolled endocrinopathies such as overt hypothyroidism or adrenal insufficiency until adequately corrected, since hormone replacement may unmask or worsen these disorders.
Intracranial hypertension and slipped capital femoral epiphysis, while not absolute contraindications, warrant caution and baseline assessment. Routine fundoscopic examination, measurement of fasting glucose, and MRI for intracranial lesions are recommended before initiation.
Somatropin can up-regulate hepatic cytochrome P450 isoenzymes, thereby accelerating clearance of substrates such as corticosteroids, sex steroids, anticonvulsants, cyclosporine, and certain antidepressants.
Dose adjustments or therapeutic drug monitoring may be required to maintain efficacy of these co-medications. Oral estrogens blunt the serum IGF-1 response, potentially necessitating higher rh-GH doses in females on hormone replacement.
Concomitant glucocorticoid therapy, even at physiological replacement levels, may antagonize the growth-promoting actions of IGF-1, especially in children with adrenal insufficiency. Coadministration with the macimorelin diagnostic test can yield false-negative results due to receptor competition.
Clinicians should counsel patients to report new medications, including non-prescription anabolic agents, as the interactive potential extends to investigational metabolic enhancers and CYP3A4 substrates.
Adverse reactions to somatropin are generally dose-related and reversible upon tapering. The most frequently reported events include injection-site erythema, edema of the extremities due to fluid retention, arthralgia, and myalgia.
Adults may experience carpal tunnel syndrome secondary to soft-tissue proliferation, whereas children can manifest benign intracranial hypertension characterized by headache and papilledema. Metabolic sequelae encompass impaired fasting glucose and progression to type 2 diabetes mellitus in susceptible individuals. Rare but serious risks comprise de-novo neoplasia or recurrence of prior malignancy, pancreatitis, and slipped capital femoral epiphysis.
Long-term surveillance studies indicate that while overall incidence is low, vigilance for second tumors, particularly meningiomas in cranial-irradiated survivors, remains prudent. Safety profiles appear comparable between compounded and commercial formulations when equivalent purity and dosing practices are employed.
Somatropin is classified as pregnancy category C; controlled human data are lacking, and animal studies show variable outcomes. Placental transfer of rh-GH increases in the third trimester as endogenous placental GH supplants pituitary secretion, but clinical significance of exogenous supplementation is uncertain.
Limited case reports reveal no consistent teratogenic pattern, yet potential for fetal growth modulation, glucose intolerance, and maternal edema necessitate a risk-benefit discussion. Routine discontinuation upon confirmation of pregnancy is common practice unless continuation is deemed essential for maternal health; in such instances, the lowest effective dose should be used with obstetric collaboration and fetal growth monitoring.
Lactation data are insufficient, though the large molecular weight of the protein suggests negligible breast-milk passage.
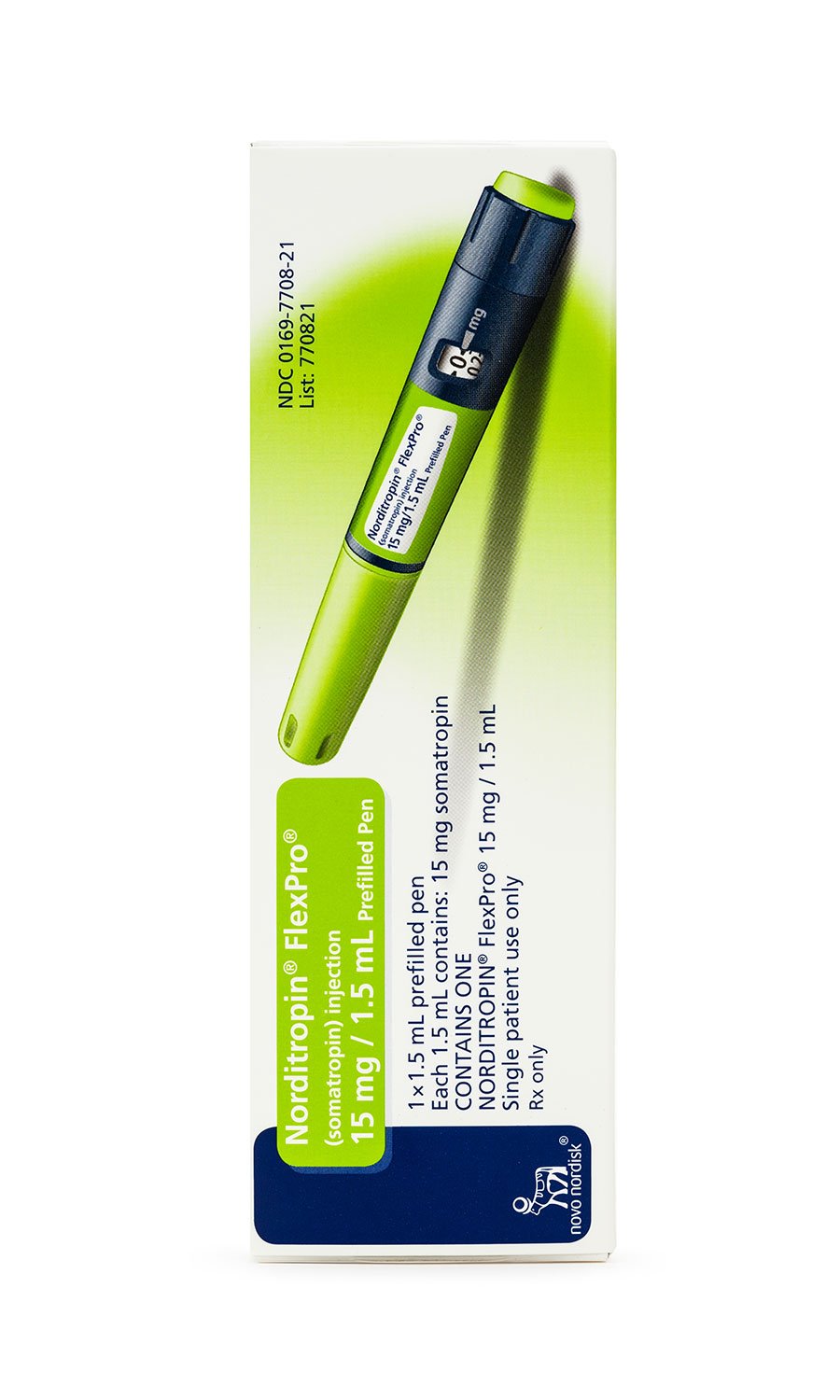
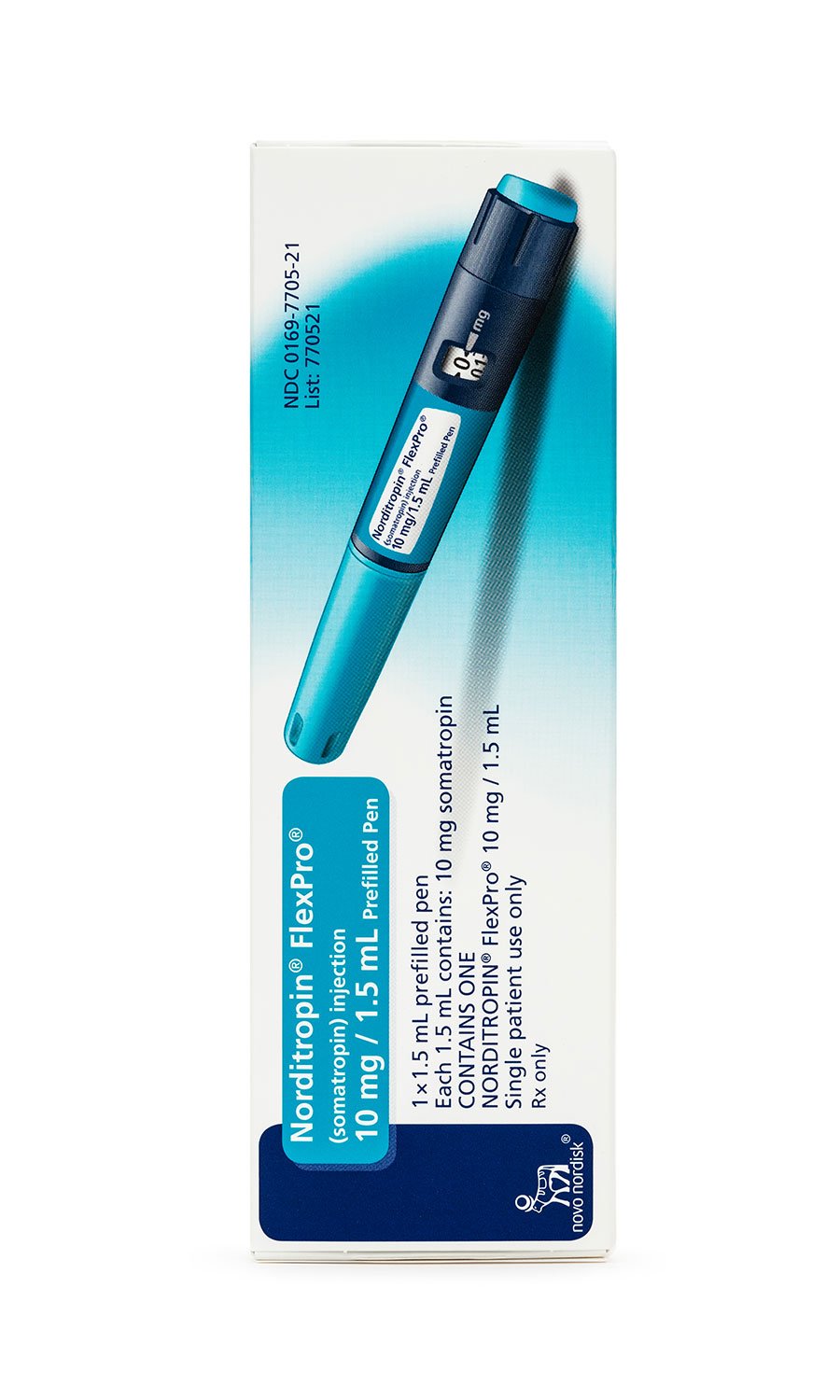
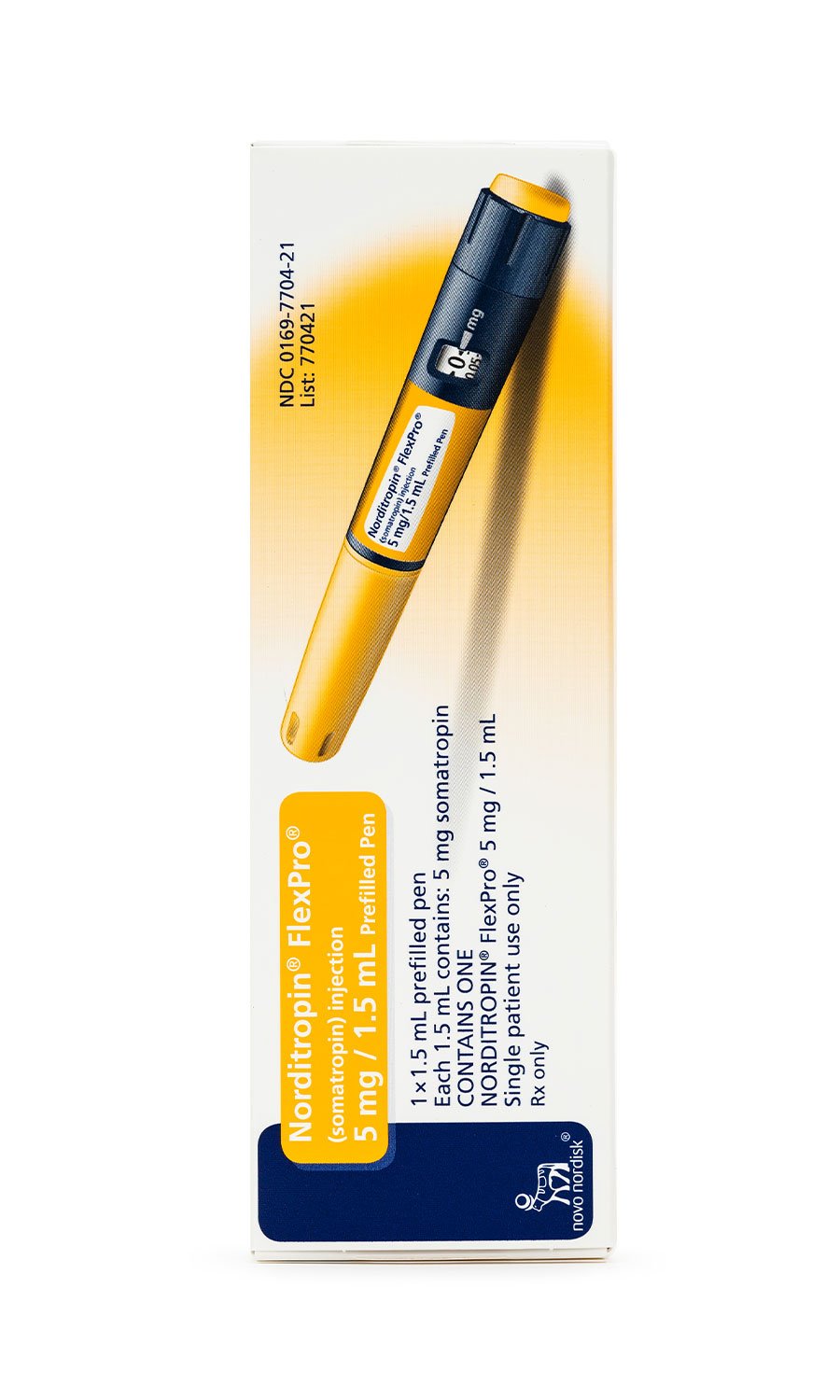
Unreconstituted Norditropin vials or pens must be refrigerated at 2 °C – 8 °C (36 °F – 46 °F) and protected from light. Compounded preparations drawn into patient-specific syringes follow identical temperature constraints.
After first use, the product may remain refrigerated for up to 28 days; excursions to ambient temperatures not exceeding 25 °C (77 °F) for a cumulative 14 days are permissible but shorten total shelf life accordingly.
Freezing irreversibly denatures the 191-amino-acid protein, while vigorous agitation predisposes to aggregation; both conditions mandate disposal. Patients should be educated to inspect the solution visually for cloudiness or particulate matter and to discard any compromised syringes.