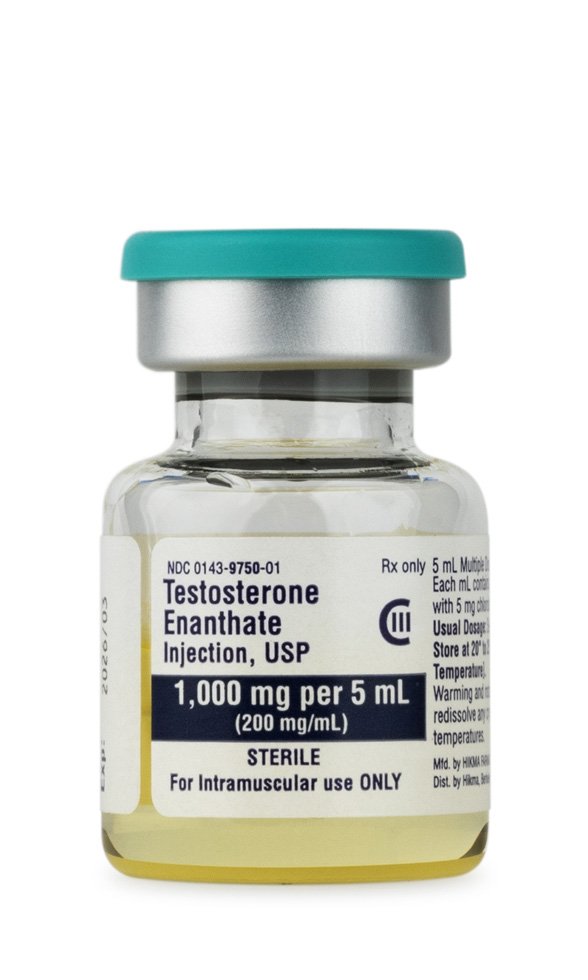

Testosterone Enanthate Injection is a compounded intramuscular androgen formulation prepared in sterile grapeseed oil at a concentration of 200 mg/mL and dispensed in multi-dose 5 mL vials for prescription-only use. It is indicated for testosterone-replacement therapy in adult males with clinically confirmed hypogonadism and for select female patients with inoperable metastatic breast cancer; all other uses remain off-label and must be justified by individualized clinical judgment. Because it is compounded under section 503A, the preparation is not evaluated by the U.S. Food and Drug Administration for safety, efficacy, or bioequivalence, and practitioners must therefore rely on primary literature, clinical guidelines, and therapeutic monitoring to mitigate risk.
Pharmacologically, the depot nature of the enanthate ester confers a prolonged release profile relative to unesterified testosterone, allowing dosing intervals of one to four weeks while still producing considerable peak-to-trough variability. Individualized titration is essential to achieve serum trough levels in the mid-normal physiologic range, thereby minimizing adverse effects such as erythrocytosis, gynecomastia due to aromatization, or suppression of endogenous spermatogenesis. Appropriate patient selection, baseline screening for prostate and breast malignancy, and ongoing surveillance of hematocrit, lipids, liver enzymes, and prostate-specific antigen are mandatory components of responsible therapy.
Typical adult male replacement regimens involve intramuscular injections of 75 to 200 mg every one to two weeks, titrated according to trough serum testosterone, hematologic indices, and clinical response. For transgender and non-binary individuals seeking masculinization, initial doses often mirror hypogonadal protocols but require multidisciplinary oversight and documentation of gender-affirming indications. Pediatric use for delayed puberty employs lower, gradually escalating doses. Compounded 200 mg/mL vials allow precise volumetric adjustments; strict aseptic technique and single-patient use of multi-dose vials are mandatory. Serum testosterone should be measured midway between injections for weekly schedules or just before the next dose for bi-weekly schedules, with target levels maintained between 400 and 700 ng/dL to minimize fluctuations.
binds intracellular androgen receptors in target tissues such as muscle, bone, skin, and the central nervous system. Ligand-bound receptors translocate to the nucleus and modulate gene transcription governing protein synthesis, erythropoietin production, and epiphyseal maturation. Peripheral metabolism yields two principal active metabolites: dihydrotestosterone via 5-alpha reductase, enhancing androgenic signaling in prostate and cutaneous tissues, and estradiol via aromatase, mediating bone mineralization and feedback inhibition of the hypothalamic-pituitary-gonadal axis.
Hepatic cytochrome P450 3A4, 3A5, and fetal-predominant 3A7 catalyze regio- and stereoselective hydroxylation, leading to urinary excretion of conjugated metabolites; variability in these pathways influences both efficacy and drug interactions. The elimination half-life of the enanthate ester following intramuscular administration averages four to five days, but residence time is extended by the oil-based depot, necessitating careful scheduling to avoid supraphysiologic peaks and subtherapeutic troughs.
Absolute contraindications include known or suspected carcinoma of the prostate or male breast, pregnancy or breastfeeding, hypersensitivity to testosterone or formulation components, and serious hepatic, renal, or cardiac impairment that could be exacerbated by fluid retention. Polycythemia (hematocrit > 54 %) warrants therapy interruption until values normalize, and untreated severe sleep apnea or uncontrolled heart failure are compelling reasons to defer treatment. Clinicians should avoid administration in patients with elevated prostate-specific antigen without urologic evaluation, and those with poorly controlled thrombophilia, since androgen-induced rises in hematocrit and platelet activation may amplify thromboembolic risk.
Androgens may potentiate the hypoglycemic action of insulin and oral antidiabetic agents, requiring dose reductions and enhanced glucose surveillance. Concomitant use with vitamin K antagonists such as warfarin can increase international normalized ratio, mandating frequent coagulation monitoring. Co-administration with systemic corticosteroids or ACTH analogues enhances sodium and fluid retention, elevating the risk of edema and exacerbating hypertension or congestive heart failure. Cytochrome P450 inducers (e.g., rifampin, carbamazepine) may accelerate hepatic clearance of testosterone, whereas strong CYP3A4 inhibitors (e.g., ketoconazole) could raise systemic exposure. Vigilance is likewise necessary with other hepatotoxic drugs to minimize cumulative hepatic burden.
Common adverse effects include acne, seborrhea, and injection-site pain, reflecting androgenic stimulation of pilosebaceous units and local tissue irritation. Systemic outcomes encompass erythrocytosis, elevated hemoglobin-hematocrit with associated hyperviscosity symptoms, reductions in high-density lipoprotein cholesterol, and potential exacerbation of hypertension. Neuropsychiatric manifestations such as mood lability, aggression, or depression have been documented, underscoring the need for mental-health screening. High-dose or illicit use has been linked to hepatotoxicity ranging from transient enzyme elevations to cholestatic jaundice or peliosis hepatis, as well as unfavorable cardiovascular outcomes in susceptible populations. Evidence on major adverse cardiac events remains conflicting, but caution is advised in individuals.
Testosterone Enanthate is contraindicated during pregnancy (formerly FDA category X) because transplacental androgen exposure can virilize a female fetus and disrupt normal genital differentiation. Animal studies reveal dose-dependent teratogenicity, and limited human data show potential for fetal growth restriction and ambiguous genitalia.
Patients of reproductive potential should employ effective contraception throughout therapy, and therapy should be discontinued well in advance of planned conception to allow hormonal washout. Breastfeeding is discouraged due to unknown excretion in milk and potential endocrine disruption in neonates
Store vials at controlled room temperature 20 – 25 °C (68 – 77 °F) and protect from light to preserve ester integrity. Do not refrigerate or freeze, as crystallization can compromise sterility and dosing accuracy. Because grapeseed oil exhibits low viscosity at room temperature, gentle warming between palms may facilitate withdrawal through a narrow-gauge needle without compromising product quality. Inspect visually for particulate matter or discoloration before each use and discard any vial exhibiting contamination or vial integrity breach.